Study Emphasizes Caution in Antipsychotic Prescriptions for High-Risk Groups

A recent case report assessed an 80-year-old man with a history of dementia, bilateral blindness, glaucoma, hearing loss, hypertension, and hypercholesterolemia complaining of visual hallucinations. Risperidone was first prescribed, followed by a combination with Quetiapine, and eventually replaced with valproate due to lack of symptom improvement and non-adherence. Three months after stopping antipsychotic medications, he developed orofacial tremors.
Researchers concluded that, when prescribing antipsychotics, physicians must be cautious of tardive dyskinesia (TD) as a potential delayed side effect, and physicians need to monitor for early signs of TD, especially in high-risk individuals. In this case, risk factors included old age, prolonged risperidone use, and abrupt cessation of the drug.
Comprehensive Study Unveils Insights into Vocal Tics: Causes, Symptoms, and Treatment Options

In a study, researchers reviewed the symptoms, causes, and treatment of vocal tics, which are characterized by involuntary verbal sounds or words ranging from subtle to pronounced. Researchers noted that tic disorders, including Tourette’s syndrome, are among the diagnostic criteria for such conditions, often originating in childhood, but possibly emerging in adulthood. Vocal tics can also accompany conditions like attention deficit hyperactivity disorder, autism, obsessive-compulsive disorder, schizophrenia, or traumatic brain injury. Some medications, including antipsychotics, anticonvulsants, and antidepressants may induce tics. Medications like aripiprazole or haloperidol, and therapy such as comprehensive behavioral intervention for tics, can help manage tics and their impact on daily life.
Debunking Myths and Highlighting Facts About Tardive Dyskinesia and Antipsychotics

A researcher unpacked several myths and facts about tardive dyskinesia (TD). The author assessed the facts about how the risk of developing TD increases the longer a patient takes an antipsychotic and the risk factors that can increase a patient’s chance of developing TD.
IMPACT-TD Scale Launched for Comprehensive Evaluation of Tardive Dyskinesia in Daily Life

In an announcement, Teva Pharmaceuticals released the IMPACT-TD Scale, a clinician-rated tool designed to help health professionals gauge the effect of tardive dyskinesia (TD) on a patient’s daily life.
Professional and Social Stigma Faced by Individuals With Tardive Dyskinesia Movements, Study Reveals
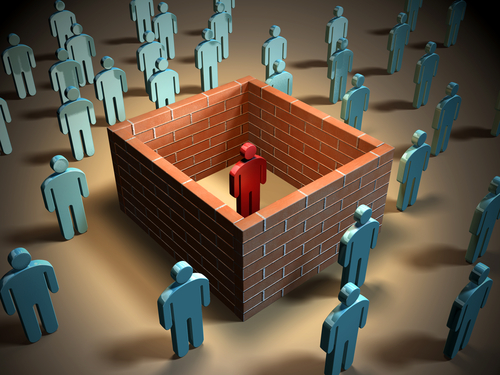
Researchers of a recent study aimed to understand the impact of tardive dyskinesia (TD) on people’s perceptions in professional and social settings. Using a randomized, blinded digital survey, participants watched a video of an actor simulating either TD movements or no TD movements, and then answered questions about employment, dating, and friendship.
Study Highlights Risk Factors and Antipsychotic Use Patterns in Patients With Bipolar Disorder and Tardive Dyskinesia

In a recent study, researchers aimed to understand the effects and patterns of tardive dyskinesia (TD+) on the quality of life and treatment results in individuals with bipolar disorder (BD). Both patients with and without TD were studied.
Emerging Synthetic Cathinones and Psychostimulant-Related Movement Disorders

Researchers of a study looked into psychostimulants, a group of substances that have effects similar to amphetamine, methamphetamine, cocaine, or cathinone, highlighting connections between psychostimulant use and movement disorders.
The researchers noted that psychostimulant-related movement disorders are a known issue seen in emergency departments worldwide. Chronic and permanent movement disorders are less commonly encountered but can manifest as a combination of symptoms such as agitation, tremor, hyperkinetic and stereotypical movements, cognitive impairment, hyperthermia, and cardiovascular dysfunction. The underlying mechanisms of these disorders involve monoaminergic signaling, particularly dopamine, but other pathways are also involved. Researchers concluded that there are common mechanisms that connect the use of psychostimulants and various movement disorders.
Unraveling Tardive Syndrome: Involuntary Movements and Sensory Complaints Persist Despite New Antipsychotic Drugs

Researchers in a recent study gathered information on tardive syndrome (TS) as TS continues to persist despite the availability of newer antipsychotic drugs. TS is a secondary syndrome resulting from the use of dopamine receptor-blocking agents, and it can manifest in different forms such as dyskinesia, dystonia, akathisia, tremors, and parkinsonism. These symptoms often persist even after discontinuing the medication and may worsen over time. Treatment options for TS involve discontinuation or replacement of the medication with atypical antipsychotics like quetiapine or clozapine. Additionally, dopamine depleters such as tetrabenazine and its derivatives (deutetrabenazine and valbenazine) are used to alleviate symptoms with fewer side effects. Deep brain stimulation of the globus pallidus internus has also shown effectiveness in treating TS, particularly when medications fail to improve symptoms.
Study Uncovers Neural Network Vulnerability in Tardive Dyskinesia’s Orofacial Symptoms

In a recent study, researchers aimed to understand why tardive dyskinesia (TD) often exhibits orofacial symptoms, while also exploring the neural network involved.
Link Between Antidepressants and Tardive Dyskinesia Explored

In a recent study, researchers critiqued various reviews and case reports associating non-dopamine-receptor-blocking drugs (DRBDs) with a tardive dyskinesia (TD) like syndrome, examining if the cases met TD criteria and excluded DRBD use. Their findings indicate that both tricyclic antidepressants (TCAs) and selective serotonin reuptake inhibitor antidepressants (SSRIs) may reveal or worsen TD in individuals previously exposed to or using DRBDs; however, they found minimal evidence supporting TD’s existence outside of this context.
