tDCS Shows Promise in Treating Tardive Dyskinesia in Patients With Schizophrenia

In this study, researchers aimed to evaluate the efficacy and safety of transcranial direct current stimulation (tDCS) in treating tardive dyskinesia (TD) in chronically hospitalized patients with schizophrenia.
Electroconvulsive Therapy for Treatment-Resistant Tardive Dyskinesia and Dystonia: Case Report and Review

This case report presents a 25-year-old female with tardive dyskinesia and tardive dystonia, which were refractory to valbenazine treatment.
Understanding Drug-Induced Movement Disorders: Risks of Antipsychotics and Anticholinergics

Antipsychotic medications are widely used for psychiatric conditions, but they are associated with significant side effects, including drug-induced movement disorders (DIMDs) like drug-induced parkinsonism, acute dystonia, tardive dyskinesia (TD), and neuroleptic malignant syndrome (NMS).
Deep Brain Stimulation and Treatment for Severe Tardive Dyskinesia
Tardive dyskinesia (TD) is typically caused by long-term use of dopamine receptor antagonists, especially neuroleptics, and can develop after months or years of medication use. The risk of developing TD is linked to the strength of a drug’s binding to dopamine receptors, with elderly patients being more susceptible.
Advances in Tardive Dyskinesia Treatment: VMAT2 Inhibitors and the Importance of Early Diagnosis

Recent advances have introduced treatment options, including VMAT2 inhibitors, for patients with tardive dyskinesia (TD), which help suppress symptoms, though they do not address the underlying causes.
Electroconvulsive Therapy: A Promising Alternative for Movement Disorders

Electroconvulsive therapy (ECT), traditionally used for psychiatric disorders, is increasingly recognized for its efficacy in managing movement disorders, even without psychiatric comorbidities.
Understanding Extrapyramidal System Dysfunction: Causes, Symptoms, and Advances in Treatment

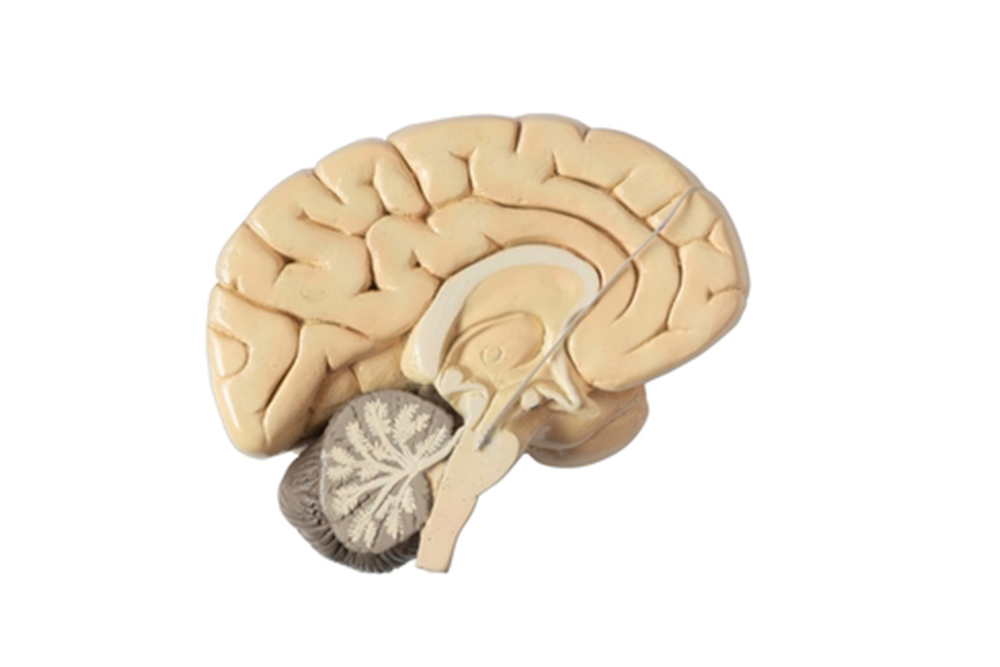
The extrapyramidal system, a complex neural network that coordinates involuntary movements and postural adjustments, plays a vital role in maintaining balance and smooth motor functioning. Centered around the basal ganglia, it fine-tunes motor signals between the cortex and thalamus, suppressing unnecessary movements.
Deutetrabenazine Proven Effective and Safe for Long-Term Tardive Dyskinesia Management

Tardive dyskinesia (TD), often associated with dopamine receptor antagonist (DRA) use, affects individuals with psychotic or mood disorders. This study evaluated the long-term efficacy and safety of deutetrabenazine, a VMAT2 inhibitor, in 343 patients through the RIM-TD open-label extension study.
VMAT1 and VMAT2 Key to Neurotransmitter Packing, Opening Avenues for Neurological Treatments

The vesicular monoamine transporters, VMAT1 and VMAT2, play crucial roles in packing neurotransmitters into synaptic vesicles, essential for neurotransmission and protecting cells from toxic cytosolic monoamines. While VMAT1 is primarily found in neuroendocrine cells, VMAT2 is predominant in the central nervous system and is implicated in various neurological and psychiatric disorders, including Parkinson’s disease and schizophrenia. VMAT2’s function in dopaminergic neurons is particularly significant, as it helps prevent oxidative stress by sequestering dopamine into vesicles, thereby reducing the production of harmful reactive oxygen species.
Managing VMAT2 Inhibitor Side Effects for Tardive Dyskinesia

At the 2021 Psych Congress Regionals, Dr. Rakesh Jain discussed the symptoms of tardive dyskinesia and provided updates on treatments, focusing on VMAT2 inhibitors. He addressed common side effects of the FDA-approved VMAT2 inhibitors, valbenazine and deutetrabenazine, and offered strategies for managing these side effects.

